Case 441
A patient, who lives in a rural region in South America, presented with bloody diarrhea and remembers having eaten undercooked pork. The attending physician submitted images to the DPDx Team of a roundworm he observed during a colonoscopy. Based on the inner structures observed which appeared to be stichocytes, Trichinella spp. was initially suspected as the causative agent. However, an ELISA test for trichinellosis was negative. Figures A-C show what was observed from the colonoscopy. What is your diagnosis? Based on what criteria?
This case and images were kindly provided by The
University of Buenos Aires, University Hospital, Parasitology Division, Buenos
Aires, Argentina.
Answer:
Whipworm (Trichuris trichiura) is contracted by ingesting the embryonated
eggs 15 to 30 days after being shed and passed with the stool (soil
contaminated hands or food). It is the
third most common roundworm to infect humans.
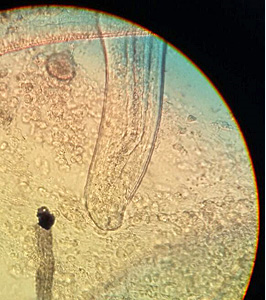
441_A - The mouth is a simple opening without lips and the oesophagus is thin, tubular and surrounded by glandular stichocytes (whole structure referred to as stichosome pharynx).
There are usually no symptoms. Although, severe
infections may cause sporadic stomach pains, bloody stools, diarrhea, and
weight loss.
441_B - Adult worms have elongate whip-like bodies (3-7cm long), with a long thin anterior end that suddenly becomes thick at the posterior end and live in the cecum and ascending colon.
The adult worms are fixed in that location, with the anterior portions threaded into the mucosa.
 |
| 441_C- Diverticulum (?); colonoscopy artifact (?) |
A 6-year-old
child from a community in rural southeastern United States presented with
severe upper right abdominal pain, fever, chills, decreased appetite and weight
loss. The child expired 2 weeks after being admitted for symptoms that
included hepatitis. At autopsy, a liver biopsy was obtained and processed.
Figures A and B show what was observed on a hematoxylin and eosin
(H & E) stained liver tissue section at 100x and 500x oil magnification
respectively. What is your diagnosis? Based on what criteria?
Answer:
C. hepatica causes a serious liver
disorder - Hepatic capillariasis.The nematode
wanders through the host liver causing tissue damage. The immune response leads
to chronic inflammation and encapsulation
of the worms in collagen fibers and consequently septal fibrosis
(abnormal connective tissue growth) and cirrhosis
of the liver. Infections of C. hepatica can present with several clinical
symptoms including, abdominal pain in the liver area, weight loss, decreased
appetite, fever and chills, hepatitis (liver inflammation), ascites
(excess fluid in the peritoneal cavity) and hepatolithiasis
(gallstones in the bile ducts).
 |
442_A - Eggs become encased by granulomatous tissue, with large sections of the parenchyma becoming replaced by these egg masses.
|
442_B - Key identification features of this parasite are a striated shell and shallow polar prominences of the egg.
|
Capillaria hepatica is rarely found in humans There are no endemic areas of infection with C. hepatica and human infection
primarily results from Zoonotic transmission. Of the human infections, most have
been found in children under the age of 5.
This parasite can be fatal in humans, as transmission and survival of the
parasite depend on death of the definitive
host in order for the eggs to reach soil and water to embryonate.

